Conclusion: USG-PNBs performed by adequately trained EPs may be a reasonable first option for analgesia during closed reduction of dislocated shoulders in the ED, particularly in patients with cardiorespiratory comorbidities. Although USG-PNBs have lower overall success for reduction, they have lower complication rates compared with PSA. This systematic review can serve as a guide for designing larger prospective studies to compare the utility of USG-PNB, IAA, and PSA for shoulder dislocation management in the ED.
Conclusions: The study found no statistically significant difference in the accuracy of US interpretation nor time spent interpreting when the pre-selected RUQ videos generated on a cart-based ultrasound machine were reviewed on a phone-sized versus a laptop-sized screen. This pilot study suggests that the accuracy of US interpretation may not be dependent upon the size of the screen utilized.
Conclusion: There was almost perfect agreement between novice practitioners and experts when determining the presence of pathologic B-lines in individual patients.
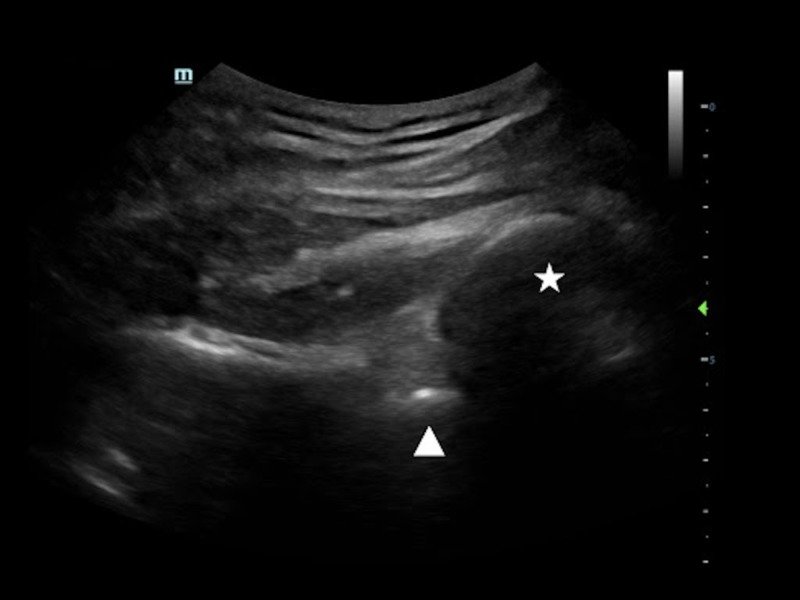
Conclusion: The presence of shoulder dislocations can be useful in distinguishing seizures from other causes of syncope. PoCUS is a useful diagnostic tool in the evaluation of both anterior and posterior shoulder dislocations.
The use of 3D printing is effective in producing a low-fidelity, ultrasound-capable model simulating an anterior shoulder dislocation. Future research will determine whether provider confidence will improve after utilizing this model and whether provider interactions with the model increases the frequency of use of intraarticular anesthesia for the management of shoulder dislocations in our department.